Background
Minimal residual disease (MRD) monitoring is an important predictor of outcomes in acute lymphoblastic leukemia (ALL), and flow cytometry is widely used to monitor MRD with a detection depth of 10 -4~10 -5. Post induction MRD is the most commonly applicated timepoint for risk stratification of ALL. About half of the patients (pts) with post induction CR/CRi achieved simultaneous MRD negativity, however, among them some pts subsequently relapse. Thus, how to better interpret the MRD results has always been a topic of interest among clinicians. Hence, in this report, we monitored MRD at different timepoints and focus on the 1-year persistent MRD negativity and its impact on the prognosis.
Method
In this prospective long-term follow-up study, we analyzed 202 cases of Ph/BCR-ABL1 negative BCP-ALL. All pts were treated with RJ-ALL 2014 protocol as follow:
The induction regimen was VDPCP, the consolidation regimen was hyper-CVAD + Pegasparagase (PEG) and the maintenance regimen was POMP + PEG. CNS prophylaxis was integrated. Pts eligible for allogeneic hematopoietic stem cell transplantation (allo-HSCT) were recommended to transplant.
MRD was monitored by 8-color flow cytometry. MRD negativity is defined as MRD < 10 -4. MRD monitoring was performed at the end-of-induction (EOI), the 3 rd month and every 3 months afterwards during 5 years. 1-year persistent MRD negativity (1-yr-MRDneg) was defined as sustained 1-year MRD negative from EOI or 3 rd month.
Results
From May 2014 to Nov 2021, a total of 202 pts were enrolled. The median age of pts at diagnosis was 35 years (range 14~65). After induction, 179 / 193 (92.7%) pts achieved CR/CRi, among them 102 (57%) pts were MRD negative (MRDneg). There were 9 (4.5%) early death during induction due to hemorrhage or infection. At the third month, 171 pts were in CR/CRi, among them, 120 (75%) of the 160 evaluable pts were MRDneg. At one year, 123 pts were in CR/CRi, among them, 48 (70.6%) of the 68 evaluable pts were MRDneg. By Jul 2023, the median follow-up time was 56 months. Ten pts were lost to follow-up. The 5-yr OS rate is 52.6% and the 5-yr RFS rate is 50.7%.
Regarding the EOI MRD status, the MRDneg group trend to have better OS (5-yr OS 63.6% vs 51.2%, p=0.128) and RFS (5-yr RFS 53.4% vs 48%, p=0.088) compare to MRD positive (MRDpos) group. Regarding the MRD status at the third month, the OS (5-yr OS 66.9% vs 38.4%, p=0.000) and RFS (5-yr RFS 64.6% vs 28.2%, p=0.000) of MRDneg group was significantly better than that of MRDpos group.
Totally, 80 pts received allo-HSCT, among them, 78 pts achieved CR and 49 pts were MRDneg before HSCT. After HSCT, 18 pts relapsed and 22 pts died, among them 7 pts died of relapse and 15 pts dead of treatment toxicity. For transplanted pts, the 5-yr OS rate is 65% and the 5-yr RFS rate is 58.6%.
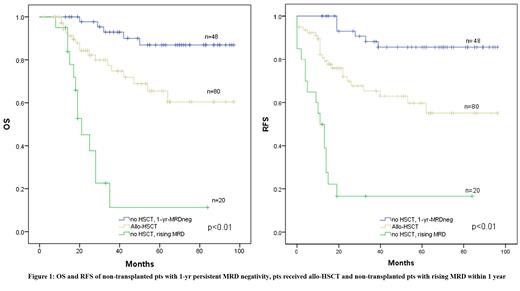
We further analyzed the 1-year persistent MRD status of non-transplanted pts. Among 113 non-transplanted pts, 68 pts had 1-year complete MRD data. Of which 48 pts had 1-yr-MRDneg and 20 pts had rising MRD within 1 year. For pts with 1-yr-MRDneg, 5-yr OS rate is 86.9% and 5-yr RFS rate is 85.7%. For pts with rising MRD, 5-yr OS rate is 11.3% and 5-yr RFS rate is 16.7%. Comparing their survival with transplanted pts we found that the OS and RFS of non-transplanted 1-yr-MRDneg pts were significantly better than allo-HSCT (OS p<0.01, RFS p<0.01), and allo-HSCT were significantly better than non-transplanted pts with rising MRD within 1 year (OS p<0.01, RFS p<0.01) (figure 1).
Conclusion
In this long-term follow-up study, we found that in Ph/BCR-ABL1 neg patients, 1-year persistent MRD negativity is a stronger prognostic predictor than EOI or 3 rd month MRD negativity. Non-transplanted pts with 1-yr persistent MRD negativity have better 5-year survival than those who receive allo-HSCT, suggesting that pts with 1-yr persistent MRD negativity may be spared from allo-HSCT.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal